Occupational and Physical Therapy Soap Note Example.
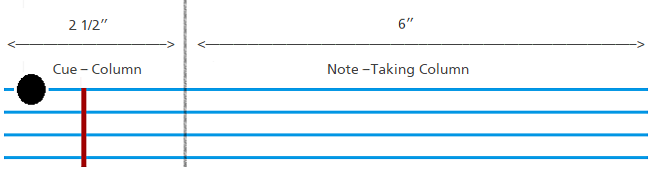
Tips on Writing a SOAP Notes To make the briefing note effective, follow the format. Make your SOAP note as concise as possible but make sure that the information you write will. Write it clearly and well-organized so that the health care provider who takes a look. Only write information that.How to Write a Progress Note (SOAP) Guides to get you through your clinical rotations year! SOAP is an acronym for Subjective, Objective, Assessment, Plan. Instead of re-writing an entire consult note, you simply being giving a quick overview of a patient’s status on specific issues at a particular period of time.Tips on Writing a SOAP Note Make sure you follow the prescribed format, you SOAP note should start from the subjective,. You SOAP not should be as clear and concise as possible. It should be well-organized so that anyone else who will pick it up will have no challenges in. Only consider.
Therapy notes (either progress notes or psychotherapy notes) may be easier to write and later to interpret if written toward a good treatment plan. Progress Notes versus Psychotherapy Notes: A Key Distinction. Psychotherapy notes. Over the years, clinicians have debated about whether it was permissible to maintain a.Progress Notes are brief narrative entries written to record negative and positive events relating to residents. They are also used to record situations regarded as irregular, and residents’ response to lifestyle issues. Progress Notes are written to supplement care documentation so that the quality of care can be continuously improved.
SOAP Notes by Cheryl Hall on August 1st, 2018. About Me. Cheryl Hall Occupational Therapist Maryland, United States. Welcome to a site devoted to sharing experience, knowledge and resources to make your job of being a great therapist a lot easier. I have been an occupational therapist for more than 30 years.